Iraq: Applying trauma systems concepts to humanitarian battlefield care: a qualitative analysis of the Mosul trauma pathway
Kent Garber,
Adam L. Kushner,
Sherry M. Wren,
Paul H. Wise & - Paul B. Spiegel
Conflict and Health volume 14, Article number: 5 (2020) Cite this article
1 Altmetric
Metricsdetails
Abstract
Background
Trauma systems have been shown to save lives in military and civilian settings, but their use by humanitarians in conflict settings has been more limited. During the Battle of Mosul (October 2016–July 2017), trauma care for injured civilians was provided through a novel approach in which humanitarian actors were organized into a trauma pathway involving echelons of care, a key component of military trauma systems. A better understanding of this approach may help inform trauma care delivery in future humanitarian responses in conflicts.
Methodology
A qualitative study design was used to examine the Mosul civilian trauma response. From August–December 2017, in-depth semi-structured interviews were conducted with stakeholders (n?=?54) representing nearly two dozen organizations that directly participated in or had first-hand knowledge of the response. Source document reviews were also conducted. Responses were analyzed in accordance with a published framework on civilian battlefield trauma systems, focusing on whether the response functioned as an integrated trauma system. Opportunities for improvement were identified.
Results
The Mosul civilian trauma pathway was implemented as a chain of care for civilian casualties with three successive echelons (trauma stabilization points, field hospitals, and referral hospitals). Coordinated by the World Health Organization, it comprised a variety of actors, including non-governmental organizations, civilian institutions, and at least one private medical company. Stakeholders generally felt that this approach improved access to trauma care for civilians injured near the frontlines compared to what would have been available. Several trauma systems elements such as transportation, data collection, field coordination, and post-operative rehabilitative care might have been further developed to support a more integrated system.
Conclusions
The Mosul trauma pathway evolved to address critical gaps in trauma care during the Battle of Mosul. It adapted the concept of echelons of care from western military practice to push humanitarian actors closer to the frontlines and improve access to care for injured civilians. Although efforts were made to incorporate some of the integrative components (e.g. evidence-based pre-hospital care, transportation, and data collection) that have enabled recent achievements by military trauma systems, many of these proved difficult to implement in the Mosul context. Further discussion and research are needed to determine how trauma systems insights can be adapted in future humanitarian responses given resource, logistical, and security constraints, as well as to clarify the responsibilities of various actors.
Background
Beginning in October 2016, the Iraqi army, supported by the Kurdish Peshmerga and a U.S.-led international coalition, launched an intensive campaign to retake Mosul, once Iraq’s second largest city, from the militant group the Islamic State, which had captured the city and much of northern Iraq and western Syria in 2014. The campaign lasted nearly nine months and became arguably the largest urban siege since World War II. Nearly one million people were displaced, and thousands killed, by the time the battle ended in July 2017 [1, 2].
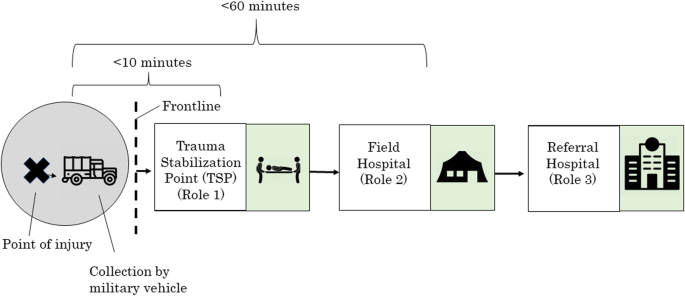
As fighting unfolded, severe gaps in trauma care for wounded civilians emerged. Humanitarian planners, led by the World Health Organization (WHO), responded by coordinating what became a novel trauma response pathway designed to improve access to trauma and surgical care. This pathway drew upon the concept of “echelons of care” used by the North Atlantic Treaty Organization (NATO) and other military evacuation systems, in which war-wounded are stabilized near the frontlines and, when necessary, transferred “up the chain” to higher levels of care [3]. In Mosul, three levels, or echelons, of care were ultimately implemented for civilians: Trauma stabilization points (TSPs), run by medical non-governmental organizations (NGOs), were situated within 10–15?min of the frontline; field hospitals were established within roughly an hour of the point of the injury; and referral hospitals for more complex injuries were designated further away from the theatre (Fig. 1).
Fig. 1
Schematic Representation of Mosul Civilian Trauma Pathway
Full size image
In many ways, this pathway represented a marked departure from “business as usual” for humanitarian trauma care in wartime. Although echelons of care are well-described in war surgery literature, they are most commonly associated with western militaries, having been deployed in military responses in Vietnam, Israel, and the Falkland Islands in the 1970s and 1980s through Afghanistan and Iraq more recently [4, 5]. These military evacuation chains provided first aid near the point of injury, transport of the critically wounded, and surgical care for combatants and, to varying degrees, injured civilians. Humanitarian actors, by contrast, have historically been constrained by resource, security, and logistical challenges and have not organized formal, military-style trauma evacuation pathways [6,7,8,9,10]. As the International Committee for the Red Cross (ICRC) noted, “echelons for the management of war wounded do not always exist in a civilian or humanitarian context”; rather humanitarians often work at a single site, at variable distances from the frontlines, and have been dependent upon the war-wounded getting to them by whatever means possible [11]. Even when echelons do exist, they are often rudimentary: In the 1980s, for example, the ICRC supported a series of “first aid posts” and field hospitals in Afghanistan and along the Afghanistan-Pakistan border, but it took patients 6–7?h, and at times more than a day, to reach one of the hospitals [7, 8]. Moreover, on principle, many humanitarian organizations feel strongly that care at or near the frontlines is -- and should remain -- the responsibility of professional militaries, not humanitarians, in accordance with the Geneva Conventions [12, 13].
Yet recent experiences in Iraq and elsewhere have shown that humanitarian agencies are actively reassessing, and seeking to improve, how they deliver trauma and surgical care [14, 15]. These efforts began with natural disaster responses, reflecting the fallout from the 2011 Haiti earthquake response that was widely criticized as slow, fragmented, and poorly coordinated [16]. Agencies are now re-examining trauma care in war, spurred in part by growing lessons from military battlefield trauma systems over the past two decades. In the 2000s, the U.S.-led international coalition in Iraq and Afghanistan made massive investments in battlefield trauma systems that have been credited with a marked reduction in servicemember fatality rates compared to previous armed conflicts [17, 18]. Critically, these systems feature not only multiple echelons of care (from point of injury to complex rehabilitative care), but also integrative components such as communication, transportation, data collection, and clinical practice guidelines that enabled a continuum of timely, quality care for the gravely injured [3, 5]. Many of these elements have been credited with saving lives, including reduced times between injury and definitive care (often through the use of air evacuation to limit the time between injury and definitive care to less than one hour); better tactical pre-hospital care that prioritized hemorrhage control including tourniquet use, resuscitation with blood products, and hypothermia management; sustained en-route care during transportation; and real-time use of data to improve care delivery [5, 19, 20]. In sum, the combination of improved data collection and analysis, clinical practice guidelines, and real-time clinical governance have enabled such achievements.
Given the novel application of military-style echelons of care to the Mosul humanitarian trauma response, as well as the growing interest from humanitarians to strengthen trauma care in conflict settings, there is a need to better understand what was done in Mosul and to examine how trauma systems insights were manifest in this approach and how they might be improved in the future. Accordingly, the purpose of this study is to analyze the Mosul trauma response through a trauma systems lens, drawing upon a published framework for civilian battlefield trauma systems [21]. This framework outlined a schema featuring multiple levels of care, with providers and activities designated at each level (Table 1); it also specifies six supportive or integrative components: coordination, communication, transportation, health information systems, education and training, and research. Applying this framework, the study aims to assess whether the Mosul trauma pathway functioned as an integrated system and to identify areas that could be strengthened, context-permitting, in future responses.